The artificial heart represents a major technological and medical achievement, having already saved many lives. The idea of replacing a failing heart with a medical device may sound like something straight out of a science fiction novel, but it is a reality that is still changing the landscape of cardiovascular medicine today. In response to evolving medical techniques, the collaboration of engineers and doctors has led to the development of several types of cardiac prosthesis since the 20th century.
The first ideas
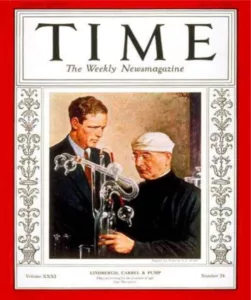
The idea of creating an artificial heart developed before the Second World War, when surgeon Alexis Carrel met American aviation pioneer Charles Lindbergh. The two men worked together to create this artificial heart in 1930, which artificially reproduces the heart-lung system by seeking to keep these organs alive using a perfusion pump, nicknamed the “glass heart”. However, physiological problems prevented the two men from succeeding.
The initial research
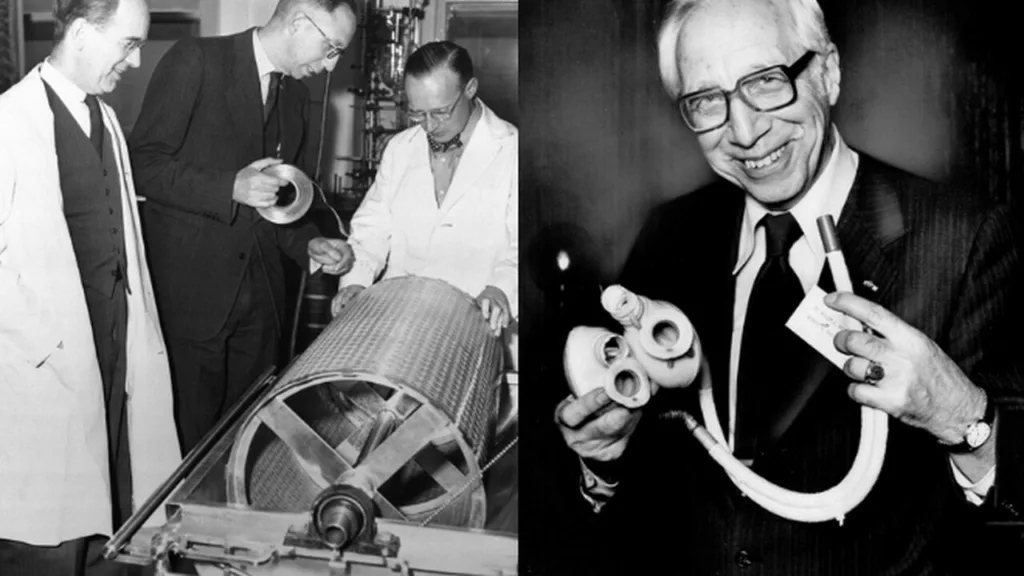
A few years later, in 1945, it was Wilhem Kolff and Tetsuzo Akutsu’s turn to take over the development of this artificial heart. A pioneer of the artificial kidney during the war, Kolff decided to work with Tetsuzo Akustu, a renowned surgeon in artificial heart development, to create and perfect the idea. Their work was based on the principle of “an artificial heart, consisting of two ventricular chambers sewn onto the atria of a fairly large animal, such as a dog. Artificial valves would separate the chambers, and a membrane driven by a pneumatic flow would empty and fill them”. In 1957, the artificial heart was born. It was implanted in the thorax of a dog, which survived 90 minutes.
The first human implants
En 1963, Domingo Liotta, chirurgien argentin et ancien élève de Kolff et Akutsu , rejoint l’équipe de recherche de Michael DeBakey, père de la médecine cardiovasculaire moderne. Liotta poursuit l’idée du cœur artificiel en s’attachant à réaliser un cœur partiel, qui remplacerait uniquement le ventricule gauche. En 1966, la pompe pneumatique est implantée chez une patiente de 37 ans. 10 jours plus tard, la pompe est retirée : c’est un succès !
En 1969, Liotta travaille avec Denton Cooley à la réalisation de la première implantation totale d’un coeur artificiel (nommé Liotta-Cooley) sur un patient de 47 ans, qui décéda quelques heures plus tard d’une infection. La procédure démontrera la viabilité des cœurs artificiels comme passerelle vers la transplantation chez les patients cardiaques.


The first total artificial hearts
In 1971, Robert Jarvik developed the Jarvik7, a polyurethane heart that was implanted in several patients. Barney Clark, the first patient, remained connected to the device for 112 days (a device that weighed 180 kilos at the time!). In 2001, Abiocor I revolutionized total cardiac prostheses by eliminating all cables (implanted batteries), but its size was too imposing to remain on the market. In 2013, Alain Carpentier inaugurated the Carmat artificial heart, after more than 20 years of research, which is now being marketed as part of clinical studies.
Although there is still a long way to go, and heart transplantation remains the reference treatment for patients with severe heart failure, the shortage of grafts justifies the need to design a new-generation artificial heart as a bridge to transplantation and as a destination therapy. Research is multiplying with the ultimate aim of creating the artificial heart that will become the treatment for heart failure!
As part of this research dynamic, Procope Medicals has been working for the past 5 years on a prototype of a total artificial heart, in collaboration with cardiac surgeons at Nantes University Hospital. Our aim is to provide patients with a better quality of life, by eliminating external transmission via cables, and creating a prosthesis available in 2 sizes, to suit all patient morphologies.
