Heart disease is the leading cause of death in both men and women, but it can develop and manifest itself very differently according to gender. Let’s explore the origins of these differences, but also the evolution of stereotypes in the conduct of epidemiological studies and the processing of figures.
Left out of the research
It wasn’t until the mid-1980s that interest began to focus on how heart disease might affect women, at which time the Framingham Heart Study, the first in-depth, long-term cardiovascular study conducted in the USA, began to report gender-specific patterns of heart disease, questioning whether the extent of this pathology in women had been overlooked, given the insufficient number of women included in the research up to that point. As heart disease was thought to affect mainly men, only men were studied.
Over 30 years ago, the US Congress called on the National Institutes of Health to include as many women as men in clinical trials. But while progress has been made, equity remains elusive. And that’s dangerous for women: “Since 2000, women in the U.S. have reported adverse events from approved drugs 52% more often than men, and serious or fatal events 36% more often,” said research firm McKinsey & Company in a report published in January 2024.
A German study showed that, despite identical technical success for men and women in percutaneous cardiac intervention, the age-adjusted risk of death or cardiac event was 20% higher in women than in men.

Inequality figures
The challenges women face when seeking healthcare manifest themselves in many ways, for different diseases and in different sectors of society.
On International Women’s Health Action Day, the association Agir pour le cœur des femmes revealed worrying data from the Observatoire national de la santé des femmes 2024, derived from Women’s Heart Bus screenings.
89% of women have at least two cardiovascular risk factors (smoking, diabetes, hypertension, sedentary lifestyle, alcohol, family history, obesity, high triglycerides).
46% have gynaecological risk factors (contraindicated contraception, lack of follow-up).
67% are affected by psychosocial factors (stress, depression).
The French Federation of Cardiology (FFC) is calling for greater awareness and management of the specific needs of women.
New approaches to combat healthcare disparities
Increasingly, global public health programs are being designed from a sex- and gender-sensitive perspective: this involves studying the role played by sex and gender in health outcomes, including health-related stigma, barriers to accessing health services and vulnerabilities to different health risks. One of the pillars of this approach is the systematic collection, analysis and use of sex-disaggregated data, and the inclusion of sex and gender in monitoring and evaluation.
Earlier diagnosis and a more holistic, patient-centred approach to treatment could also help to improve disease and symptom management, prevent uncontrolled progression and related complications, and reduce unnecessary or inappropriate treatment.
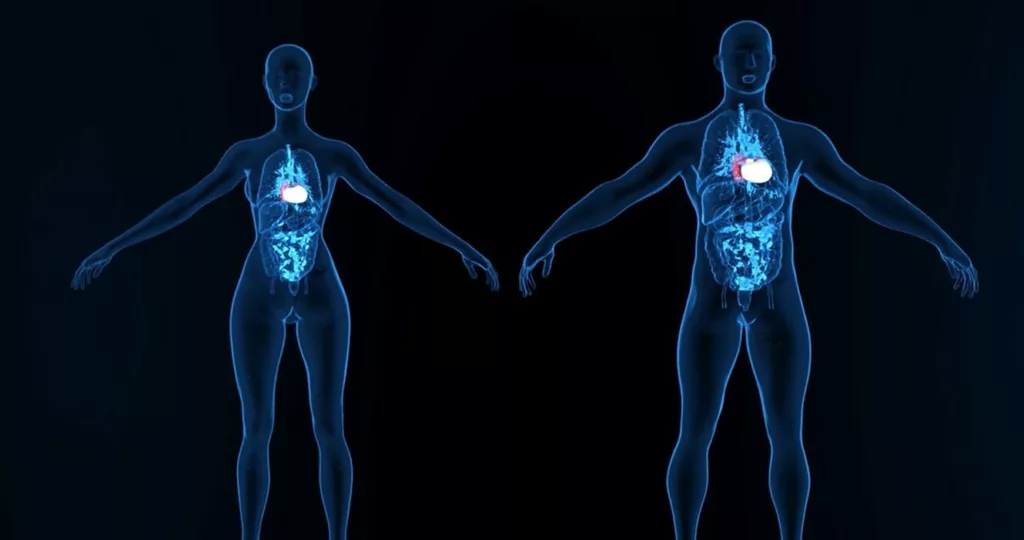
PROCOPE Medicals has designed an innovative cardiac device based on pneumatic technology protected by an international patent. The disruptive nature of the device, compared with what already exists, lies first and foremost in optimizing the size of the prosthesis: 2 volumes (50cc and 70cc) to ensure maximum morphological compatibility (currently, some devices are only compatible with 65% of men and less than 20% of women).
Sources :
https://www.who.int/fr/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds)
https://www.nhlbi.nih.gov/science/framingham-heart-study-fhs
https://time.com/6962474/heart-disease-research-women/
https://www.futura-sciences.com/sante/actualites/maladies-cardiovasculaires-89-femmes-seraient-haut-risque-cardiovasculaire-113721/
