Heart transplantation is the reference treatment for patients suffering from severe heart failure, whose main challenge is to cope with the shortage of organs: “On average, there are two compatible recipient candidates for just one available heart graft”, explained Doctor Guihaire in 2021.
But what is the current heart transplant landscape in France? What about the selection of recipient candidates? And what are the prospects for the future?

Heart transplant figures
In 2019, 425 heart transplants were performed in France, and 411 in 2022. While this number is declining year on year and remains low compared with the number of candidates waiting for a graft (2 to 1), the rate of heart transplants in France nevertheless remains higher than many other countries.
Also in 2019, 573 new candidates were placed on the waiting list. On average, 13% of patients on the waiting list die, for want of a transplant, in the year following their registration. The role of the Agence of Biomédecine is to manage a national waiting list and the allocation of transplants.
The heart is a fragile organ, and the number of grafts in good condition is far lower than the need.
The problem has become more acute over the years, as the criteria for graft selection have become increasingly specific. Indeed, there are many risk factors originating from the donor, which will have an impact on the recipient’s survival after transplantation.
How are candidates for heart transplantation determined?
The distribution of heart transplants is therefore a challenge, given the scarcity of this vital resource. In France, equitable graft allocation is necessary to guarantee fair and efficient access to heart transplantation. Until 2004, the allocation process was based on a concentric territorial logic, whereby grafts were allocated to heart transplant centers according to regional and national criteria.
The need to adapt allocation rules to patients’ changing clinical needs, and to ensure a more equitable distribution of heart transplants throughout France, prompted the creation of the Heart Score.


A Heart Score for better allocation
The Heart Score was introduced in 2017 by the Agence de Biomédecine to ensure a fair and legitimate distribution of heart transplants, it takes into account hemocompatibility as well as geographical pattern, i.e. the travel time between the donor site and the transplant site.
In addition, before being placed on the waiting list for a donor heart, each patient undergoes an in-depth assessment based on the following criteria in particular:
– Determination of blood type : The donor’s blood type and that of the recipient need not be identical (A, B, AB and O), but must be compatible.
– Thorough tissue characterization (HLA characterization) : Tissue proteins are present on almost every cell in the human body, and each individual has a unique combination of tissue proteins. The greater the compatibility between the donor’s tissue proteins and those of the recipient, the lower the risk of rejection.
– Assessing the risk of infection after transplantation : it is vital to identify certain chronic infections in good time and treat them if necessary. After transplantation, patients receive drugs that suppress the immune system, making them more vulnerable to infection.
What are the future prospects for heart transplantation ?
Today, post-transplant survival has improved over the last few decades, with an 80% survival rate after 1 year of transplantation.
The leading causes of death after heart transplantation are graft dysfunction, followed by infection, after one year and beyond.
What about future prospects for improvement?
– For donors, the challenge is to increase the number of donations and raise public awareness of organ donation.
– For heart transplants, the aim is to improve preservation with perfusion machines.
– For recipients, the aim is to move towards personalized medicine, with follow-up tailored to each patient.
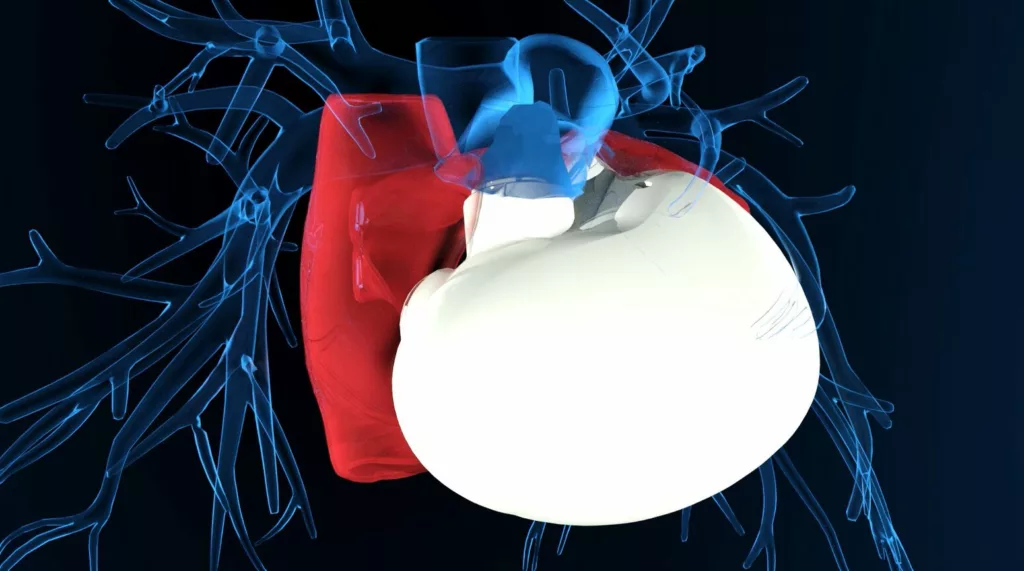
Among the treatments being considered to alleviate the shortage of transplants is the alternative of the total artificial heart. Like heart transplantation, this mechanical device is designed to completely replace failing heart function. Surgically implanted, it provides long-term circulatory support, regardless of donor availability. This solution could reduce dependence on grafts and prolong the survival of patients awaiting transplantation.
Procope Medicals is currently designing a new generation of total artificial heart, which will ultimately help to overcome this shortage and significantly improve patients’ quality of life.
Sources :
https://www.coeurassistance.com/transplantation-dons-organes
https://www.agence-biomedecine.fr/IMG/pdf/guide_score_coeur_2018.pdf
https://www.univadis.fr/viewarticle/france–parcours-et-profil-des-transplantes-cardiaques
https://www.youtube.com/watch?v=Mbj6WUZ0Xl0
Article sur la répartition des greffons cardiaques par Pascal LEPRINCE, 2017
